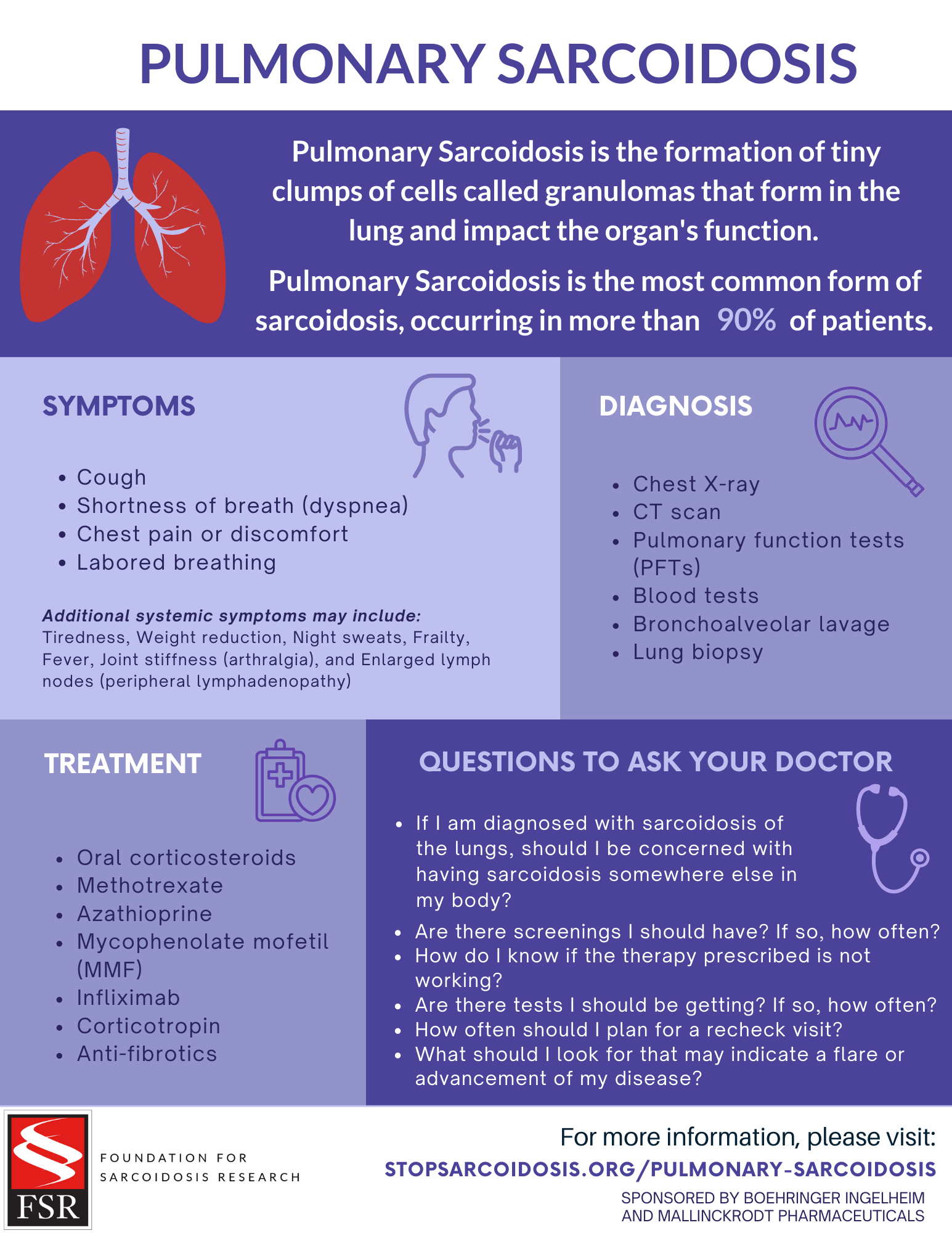
Sarcoidosis of the Lungs (Pulmonary Sarcoidosis)
Symptoms1-2
Additional systemic symptoms may include:
- Tiredness
- Weight reduction
- Night sweats
- Frailty
- Fever
- Joint stiffness (arthralgia)
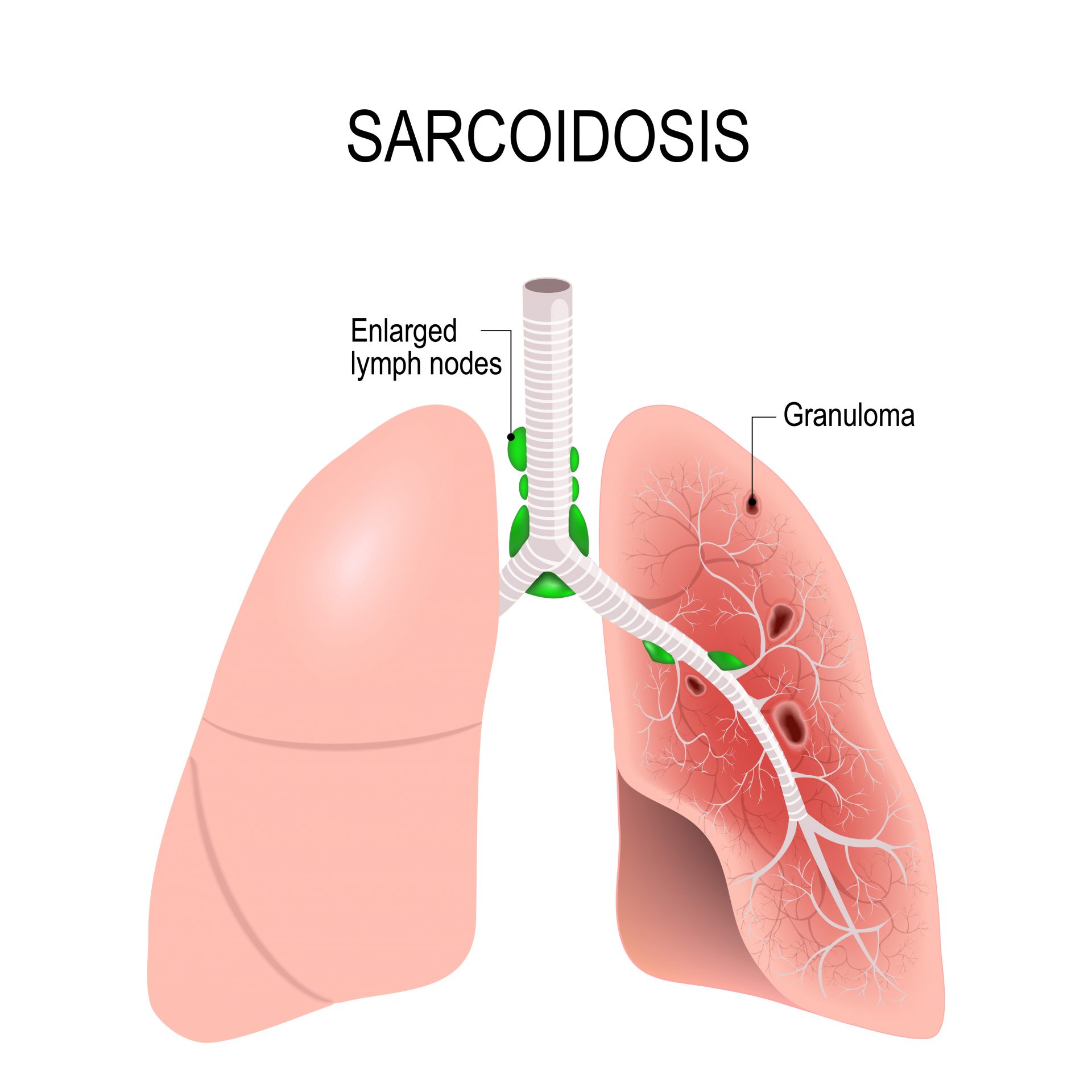
- Enlarged lymph nodes (peripheral lymphadenopathy)
Lofgren Syndrome: 1-2
Some patients may experience Lofgren Syndrome, an acute form of sarcoidosis involving swollen fat under the skin causing bumps and patches that look red or darker than surrounding skin (erythema nodosum), bilateral enlargement of the lymph nodes in the chest (hilar lymphadenopathy), fever, and ankle arthritis. These symptoms typically go away within approximately 6 weeks, though the enlarged lymph nodes typically return to normal within approximately 1 to 2 years.
Diagnosis
Pulmonary Sarcoidosis is diagnosed through a culmination of phenotypic (how the disease presents) presentations gathered through medical history, physical exam and diagnostic testing.
Sarcoidosis is a diagnosis of exclusion, which means that other disease will often have to be ruled out first before your diagnosis of sarcoidosis can be confirmed.
Your clinician may order the following diagnostic tests prior to your diagnosis. These tests may include:
-
- Chest X-ray. Chest X-rays allow clinicians to take an image of the lungs, heart, and chest cavity. Sarcoidosis my appear on an x-ray as enlarged lymph nodes in the central part of the chest, scarring of the lungs (known as fibrosis), shadowing, or haziness through the arteries and vessels.5
- CT scan. CT’s use a combination of s X-rays and computer technology to provide a more detailed image of the lung. These are often ordered to help rule out infections – like tuberculosis or aspergilloma – or cancers – like lymphedema. CTs are also helpful in determining how significantly the lung function may be impaired.6
- Pulmonary function tests (PFTs). PFT’s are used to assess a patients forced vital capacity (FVC), which measure how well a patient is able to exhale and clear the lungs of carbon dioxide and may demonstrate the pattern of difficulty breathing in or out.7
- Blood tests. There are a number of blood tests that may be ordered as part of your diagnostic work-up. Blood tests my seek to identify increase calcium, creatinine, alkaline phosphatase (ALP) among other abnormalities.8
- Bronchoalveolar lavage. This is a procedure in which a sterile saline solution is put into the lungs through a bronchoscope and then suctioned out. This solution is then tested to measure the CD4/CD8 ratio in bronchoalveolar lavage fluid, which may help to indicate the presence of sarcoidosis.9
- Lung biopsy. Through a flexible fiberoptic bronchoscopy a small piece of tissue will be analyzed. If “non-necrotizing granulomas” are found and all other causes of granulomas are ruled out, doctors will use this information and the other information to determine the sarcoidosis diagnosis. 10
- CT scan. CT’s use a combination of s X-rays and computer technology to provide a more detailed image of the lung. These are often ordered to help rule out infections – like tuberculosis or aspergilloma – or cancers – like lymphedema. CTs are also helpful in determining how significantly the lung function may be impaired.6
- Chest X-ray. Chest X-rays allow clinicians to take an image of the lungs, heart, and chest cavity. Sarcoidosis my appear on an x-ray as enlarged lymph nodes in the central part of the chest, scarring of the lungs (known as fibrosis), shadowing, or haziness through the arteries and vessels.5

Treatments
There is no cure for pulmonary sarcoidosis, at this time. Depending on the severity of the disease and the patient’s responsiveness to treatment there are a number of medications used to treat sarcoidosis. Not all patients will require treatment and some patients. The course of treatment will vary from patient to patient.
Advanced Pulmonary Sarcoidosis
Advanced sarcoidosis impacts a small portion of those diagnosed with sarcoidosis.18 However, all diagnosed with pulmonary sarcoidosis should be aware of symptoms of advanced sarcoidosis as early treatment is critical to improve survival chances. Advanced forms of pulmonary sarcoidosis include advanced pulmonary fibrosis (ILD) and pulmonary hypertension. 19
Interstitial Lung Disease (ILD)
Interstitial lung disease (ILD) refers to scarring of lungs, or lung fibrosis, which can make it increasingly more difficult to breathe. This is also referred to as pulmonary fibrosis.* ILD symptoms include shortness of breath (especially with exercise), extreme fatigue, and weight loss.
Sarcoidosis Associate Pulmonary Hypertension
Pulmonary hypertension type of high blood pressure that affects the arteries in the lungs and heart. Sarcoidosis Associated pulmonary hypertension (SAPH) is tied to difficulty breathing, low concentration of oxygen in the blood, cough, chest pain, palpitations, and heart failure.20
*Note: Pulmonary fibrosis, which is defined by scarring of the lungs is not the same as Idiopathic Pulmonary Fibrosis, which is when the cause of the scarring is unknown.

Questions to ask your doctor
- If I am diagnosed with sarcoidosis of the lungs, should I be concerned with having sarcoidosis somewhere else in my body?
- Are there screenings I should have? If so, how often?
- How do I know if the therapy you prescribed is not working?
- Are there tests I should be getting? If so, how often?
- How often should I plan for a recheck visit?
- What should I look for that may indicate a flare or advancement of my disease?
Watch Overview: Pulmonary Sarcoidosis
Sources
1.Belperio JA, Shaikh F, Abtin FG, et al. Diagnosis and Treatment of Pulmonary Sarcoidosis: A Review. JAMA.2022;327(9):856–867.
2.Jain R, Yadav D, Puranik N, Guleria R, Jin JO. Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments. J Clin Med. 2020 Apr 10;9(4):1081.
3.Cozier YC, Berman JS, Palmer JR, Boggs DA, Serlin DM, Rosenberg L. Sarcoidosis in black women in the United States: data from the Black Women's Health Study. Chest. 2011 Jan;139(1):144-50.
4.Arkema EV, Cozier YC. Sarcoidosis epidemiology: recent estimates of incidence, prevalence and risk factors. Curr Opin Pulm Med. 2020 Sep;26(5):527-534.
5.Dhakshinamoorthy Ganeshan , Christine O. Menias, Meghan G. Lubner, Perry J. Pickhardt, Kumaresan Sandrasegaran, Sanjeev Bhalla (2018). “Sarcoidosis from Head to Toe: What the Radiologist Needs to Know. Radiographics: Volume 38; Number 4. https://doi.org/10.1148/rg.2018170157
6.Ibid.
7.Rissmiller Richard W and W. Ennis James (2018). Pulmonary function testing and sarcoidosis: A review. Lung and Breath Journal. Volume 2(1): 1-5. DOI: 10.15761/LBJ.1000121
8.Elliott D. Crouser*, Lisa A. Maier*, Kevin C. Wilson*, Catherine A. Bonham, Adam S. Morgenthau, Karen C. Patterson, Eric Abston, Richard C. Bernstein, Ron Blankstein, Edward S. Chen, Daniel A. Culver, Wonder Drake, Marjolein Drent, Alicia K. Gerke, Michael Ghobrial, Praveen Govender, Nabeel Hamzeh, W. Ennis James, Marc A. Judson, Liz Kellermeyer, Shandra Knight, Laura L. Koth, Venerino Poletti, Subha V. Raman, Melissa H. Tukey, Gloria
E. Westney, and Robert P. Baughman; on behalf of the American Thoracic Society Assembly on Clinical Problem (2020). Diagnosis and Detection of Sarcoidosis An Official American Thoracic Society Clinical Practice Guideline. American Journal of Respiratory and Critical Care Medicine Volume 201 Number 8.
9.Yongchun Shen, Caishuang Pang, Yanqiu Wu, Diandian Li, Chun Wan, Zenglin Liao, Ting Yang, Lei Chen, Fuqiang Wen, Diagnostic Performance of Bronchoalveolar Lavage Fluid CD4/CD8 Ratio for Sarcoidosis: A Meta-analysis (2016) EBioMedicine,Volume 8.
10.John A. Belperio, MD; Faisal Shaikh, MD; Fereidoun G. Abtin, MD; Michael C. Fishbein, MD; S. Samuel Weigt, MD; Rajan Saggar, MD; Joseph P. Lynch III, MD (2022). Diagnosis and Treatment of Pulmonary Sarcoidosis – A Review. JAMA. 2022;327(9):856-867. doi:10.1001/jama.2022.1570
11.Kahlmann V, Moor CC, Veltkamp M, Wijsenbeek MS. Patient reported side-effects of prednisone and methotrexate in a real-world sarcoidosis population. Chron Respir Dis. 2021 Jan-Dec;18:14799731211031935. doi: 10.1177/14799731211031935. PMID: 34569301; PMCID: PMC8477709.
12.Baughman RP, Lower EE. A clinical approach to the use of methotrexate for sarcoidosis Thorax 1999;54:742-746
13.Alicia Gerke. Treatment of Sarcoidosis: A Multidisciplinary Approach. Front. Immunol., 19 November 2020
Sec. Inflammation https://doi.org/10.3389/fimmu.2020.545413
14.Ibid.
15.Baughman RP, Drent M, Kavuru M, Judson MA, Costabel U, du Bois R, Albera C, Brutsche M, Davis G, Donohue JF, Müller-Quernheim J, Schlenker-Herceg R, Flavin S, Lo KH, Oemar B, Barnathan ES; Sarcoidosis Investigators. Infliximab therapy in patients with chronic sarcoidosis and pulmonary involvement. Am J Respir Crit Care Med. 2006 Oct 1;174(7):795-802. doi: 10.1164/rccm.200603-402OC. Epub 2006 Jul 13. PMID: 16840744.
16.Robert P. Baughman, Joseph B. Barney, Lanier O'Hare, Elyse E. Lower,
A retrospective pilot study examining the use of Acthar gel in sarcoidosis patients,
Respiratory Medicine, Volume 110, 2016 https://doi.org/10.1016/j.rmed.2015.11.007.
17.Judson MA. Developing better drugs for pulmonary sarcoidosis: determining indications for treatment and endpoints to assess therapy based on patient and clinician concerns. F1000Res. 2019 Dec 30;8:F1000 Faculty Rev-2149. doi: 10.12688/f1000research.20696.1. PMID: 31942239; PMCID: PMC6944258.
18.Rohit Gupta , Marc A. Judson , and Robert P. Baughman. Management of Advanced Pulmonary Sarcoidosis. American J of Resp and Critical Care. Volume 205, Issue 5
19.Ibid.
20.Diaz-Guzman E, Farver C, Parambil J, Culver DA. Pulmonary hypertension caused by sarcoidosis. Clin Chest Med. 2008 Sep;29(3):549-63, x. doi: 10.1016/j.ccm.2008.03.010. PMID: 18539244; PMCID: PMC2593121.