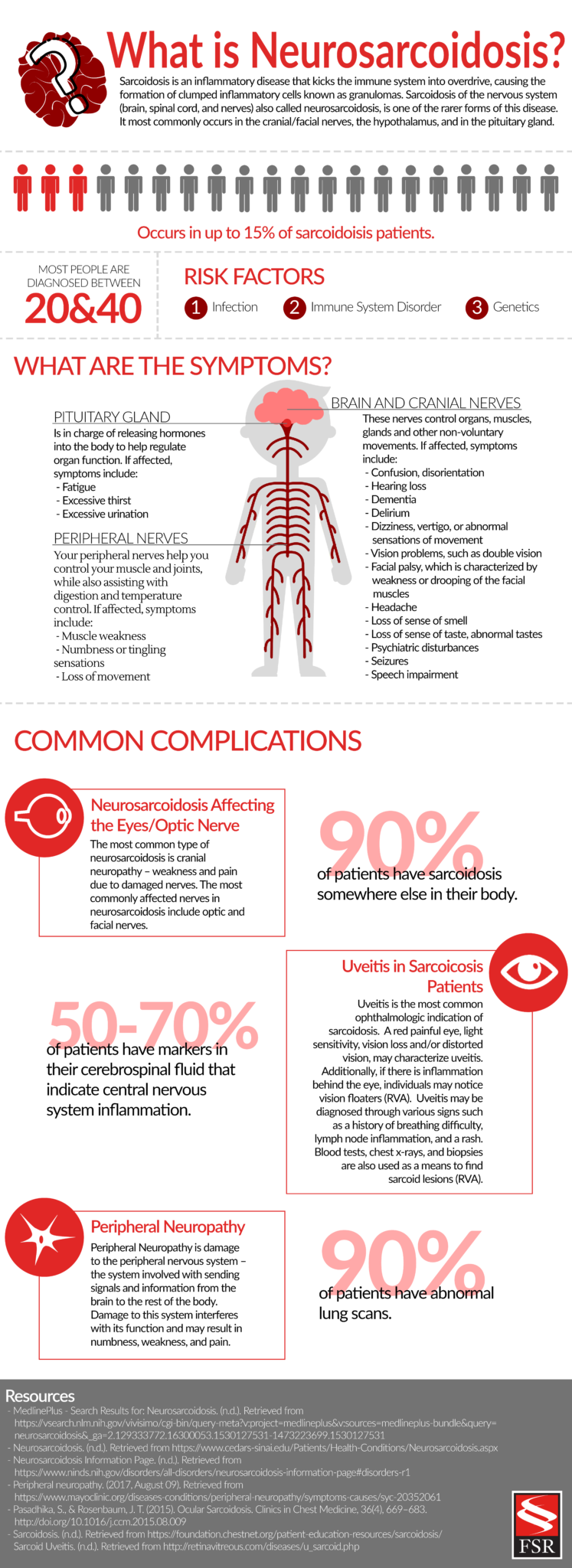
What is Neurosarcoidosis?
What Are the New Diagnostic Criteria for Neurosarcoidosis?
Below is summarized information from the criteria released by the NCCC, and created by consensus between key leaders in the field. This information can be useful to anyone who is going through the process of being diagnosed with neurosarcoidosis and their physician.
-
Many things can cause granulomas, so it is critical to rule out all other possibilities
-
Cerebrospinal Fluid (CSF) can help confirm the presence of inflammation and rule out other diseases
-
-
Between 50% and 70% of neurosarcoidosis patients have signs of central nervous system inflammation
-
These signs can include:
-
Elevated protein
-
Lymphocyte predominant pleocytosis
-
Oligoclonal bands
-
Elevated immunoglobulin G (IgG) index
-
-
- If the doctor suspects central nervous system (CNS) sarcoidosis they should do the following:
-
A magnetic resonance imaging (MRI) of the brain and/or cervical, thoracic, or lumbar spine
-
A comprehensive analysis of cerebrospinal fluid
-
-
If a doctor suspects peripheral nervous system (PNS) sarcoidosis they should do the following:
-
Electromyogram (EMG)
-
Nerve conduction study (NCS)
-
Nerve of muscle biopsy if clinically needed
-
If a physician suspects a patient may have neurosarcoidosis, they should also look for sarcoidosis in other areas of the body while conducting neurological tests.
Things to keep in mind when looking for systemic sarcoidosis:
-
Evidence of systemic sarcoidosis may not show up until later in the disease course
-
In a study of 1088 patients with neurosarcoidosis, only 31.1% initially presented with systemic symptoms, but eventually, 84% did develop systemic symptoms
-
-
Nearly 90% of patients show signs of sarcoidosis in the lungs, skin, and joints
-
Physicians should conduct a tissue biopsy of a non-neural site to confirm multi-system sarcoidosis
-
Up to 90% of patients show abnormalities on chest scans
-
If the x-rays of a patient who is highly suspected to have neurosarcoidosis comes back clean, the doctor should perform a high-resolution computed tomography (CT) scan, preferably with contrast
-
A Possible, Probable, or Definite Diagnosis
The new diagnostic criteria for neurosarcoidosis also means when patients are diagnosed with neurosarcoidosis, they will now be given a diagnosis in one of three categories; possible, probable or definite. All three of these diagnoses require the following:
- It must seem to be neurosarcoidosis and diagnostic evaluations must also suggest neurosarcoidosis
- Patients mush have an MRI, CSF, and/or EMG/NCS that shows granulomatous inflammation of the nervous system
- All other possible causes ruled out
For possible neurosarcoidosis there is no pathologic confirmation of granulomatous disease. For probable neurosarcoidosis, there is confirmation of systemic granulomatous disease consistent with sarcoidosis. Lastly, for definite neurosarcoidosis, nervous system symptoms are consistent with neurosarcoidosis and there is either evidence of sarcoidosis outside of the nervous system or no evidence because the sarcoidosis is only in the central nervous system. These three different categories “emphasize the need for the clinician to maintain an open mind” when diagnosing patients. Additionally, the Committee believes that anyone who fits into these three categories will likely receive treatment for neurosarcoidosis.