Sarcoidosis is a rare disease, affecting an estimated 150,000-200,000 Americans. Most people have never even heard of sarcoidosis, and many who have don’t know all the facts. There is a lot of misinformation about sarcoidosis out there, even within the medical community. One of our goals is to raise awareness about sarcoidosis, and that means putting an end to harmful misconceptions about the disease. Here are some of the myths about sarcoidosis that we hear most often.
“Sarcoidosis is not a lifelong illness”
60-70% of people diagnosed with sarcoidosis will go into remission without treatment. However, for the remainder of patients, the disease persists or reappears after remission. If sarcoidosis lasts longer than 3-5 years, it is considered chronic, and the symptoms can be debilitating. Some people even live with sarcoidosis their entire lives, and in rare cases, it is life-threatening. Since there is no cure for sarcoidosis, doctors often do not treat it, and instead they monitor the disease closely to ensure that the patient is not facing life-threatening risks. They monitor the disease with the hope that it will go away on its own, which is more likely but not guaranteed.
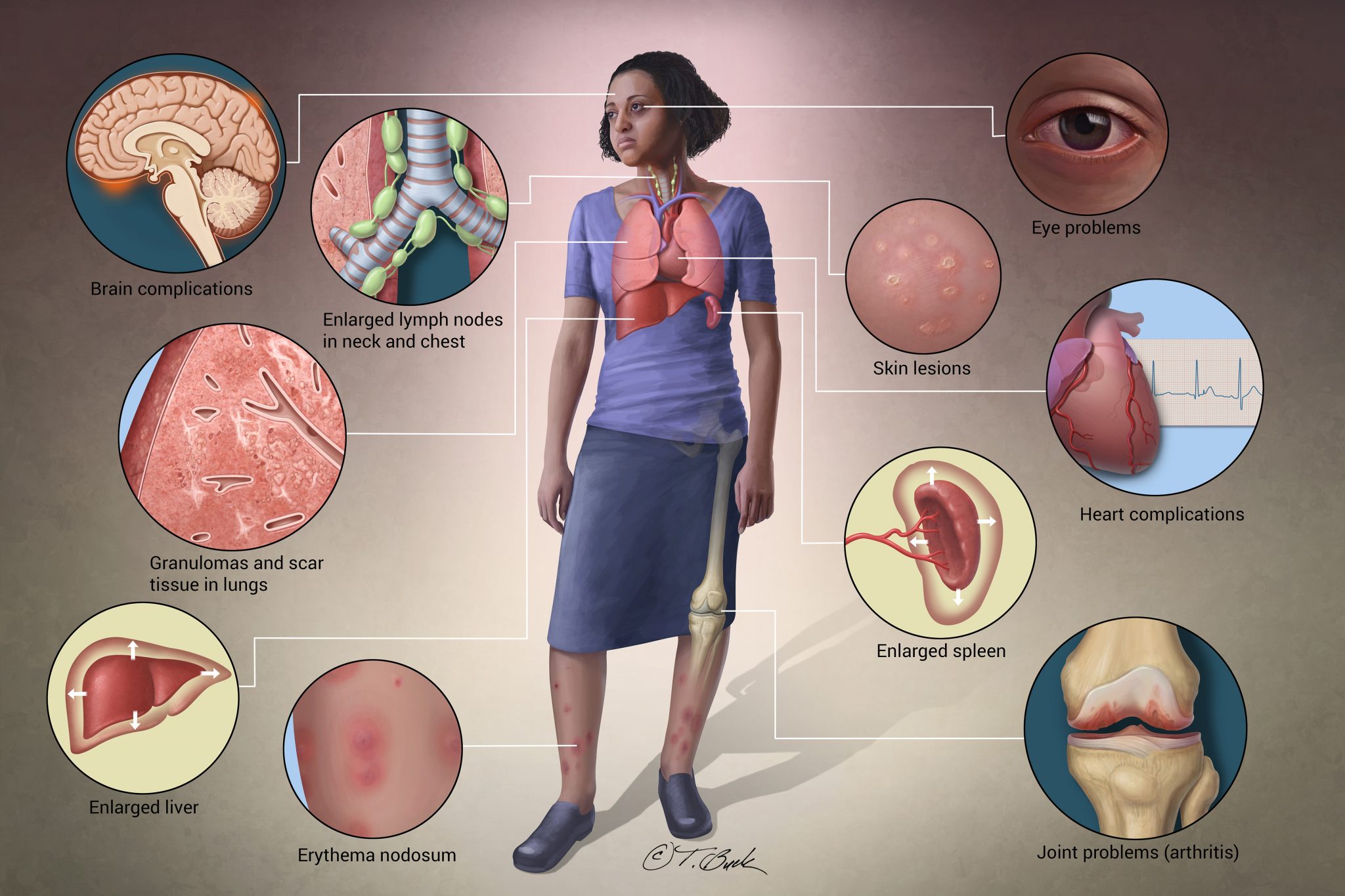
“Sarcoidosis only affects the lungs”
90% of sarcoidosis cases have lung involvement, however, sarcoidosis can affect almost any organ in the body. Symptoms can vary based on the organ that is being affected, which is one of the reasons that sarcoidosis is so difficult to diagnose. A chest x-ray alone may not catch sarcoidosis if it is not pulmonary. Sarcoidosis can affect the heart, brain, lymph nodes, skin, sinuses, and other organs. Because of this, there are many different tests that can be administered in order to diagnose someone with sarcoidosis.
“Sarcoidosis doesn’t need to be treated”
In an estimated 60% of cases, sarcoidosis goes away on its own. However, the remaining patients will require treatment. This decision is based on the risk that the disease is posing to the patient’s health and safety as well as the patient’s quality of life. If a patient is at risk of major scarring on his or her organs, or if the patient is suffering from debilitating pain, fatigue, or other symptoms, there are a number of medications that a doctor can prescribe. Unfortunately, many of these medications come with severe side effects, and some patients opt-out of receiving treatment if they feel that the side effects of the drugs are worse than the symptoms of the disease. However, some people face fatal risks if they do not receive treatment. A corticosteroid like prednisone is the most common first-line therapy prescribed to sarcoidosis patients.
“By better defining the mechanisms that cause sarcoidosis, including the role of inflammation, immune over or under-reactivity and autoimmunity, we may be better able to treat patients with sarcoidosis and maybe one day, even prevent the disease.”
“Sarcoidosis is an autoimmune disorder”
This topic has sparked a lot of debate in the sarcoidosis community. Our Scientific Advisory Board concluded that sarcoidosis is an inflammatory disorder, not an autoimmune disorder. In a patient with sarcoidosis, the immune system overreacts to something and recruits inflamed cells to combat it. This overreaction results in too many inflamed cells in one area, forming harmful granulomas. In an autoimmune disorder, a person’s immune system attacks his or her own “self” proteins, which are healthy cells.
“You’re lucky it’s just sarcoidosis”
Many people who are diagnosed with sarcoidosis must first be tested for multiple other diseases. Sarcoidosis is a diagnosis of exclusion, so doctors will rule out other diseases first. Sarcoidosis is often misdiagnosed as lymphoma because the granulomas look like cancerous masses in an x-ray. Patients have reported that when they were diagnosed with sarcoidosis, their doctors told them, “Good news, it’s just sarcoidosis.” However, sarcoidosis can turn into a chronic illness and have a severe impact on a person’s quality of life. It is life threatening in some cases, yet it is widely viewed as “not that serious” in the medical community.
There is a lot of misinformation going around about sarcoidosis. Even your doctor may not be giving you the right information. Since sarcoidosis is a rare disease, people who are well-informed about sarcoidosis are hard to find. You can use our FSR physician finder to find a doctor in your area that has experience and interest in sarcoidosis.